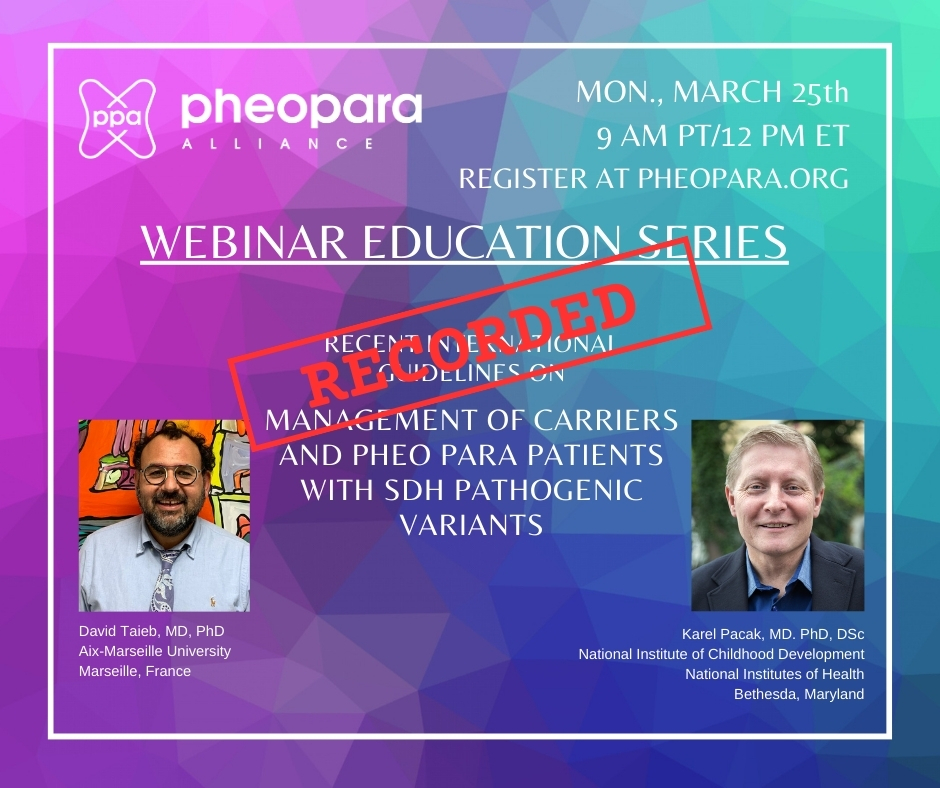
Dr. Karel Pacak, NIH & Dr. David Taieb, Aix-Marseille University
The information presented on this webinar is for educational purposes only and should not substitute the advice of your doctor(s) and medical team because they have in depth knowledge of your medical history and current situation.
View slides from this presentation here.
Questions and timing are below.
Q 1 at 40:56 “Which type of panel is the best for testing for all variants of SDHx, as well as others?”
Q 2 at 42:43 “Across the genetic variants, what is the risk of ascertainment bias? If genetic variants have largely been detected from people with clinical symptoms, how many variants may be out there but clinically silent?”
Q 3 at 44:25 “Would the germline and somatic SDHx mutation be different?”
Q 4 at 45:45 “Any evidence that following a particular diet is better for preventing tumor development in folks with SDH pathogenic variants?”
Q 5 at 47:04 “Can the SDHB mutation skip generations? I am one of 7. All of us have SDH-B although only one of our parents had SDH-B. Is that common, or unusual?”
Q 6 at 48:18 “Are there any updates to SDHB Carney Triad?”
Q 7 at 49:29 “We just had our first baby; dad has SDHB gene (and paraganglioma — glomus jugulare). How should we proceed on timing re: testing our son for the gene and surveillance if he also has it? Timing and next steps”
Q 8 at 50:53 “What are screening recommendations for maternally-inherited SDHD?”
Q 9 at 53:10 “Newly diagnosed with bilateral CBT, from inherited SDHD gene mutation. How important is it that my healthcare team has specific experience with this type of tumor? Is it safe to move forward with a team comprised of an experienced ENT and Endocrinologist (not specific experience with this tumor)?”
Q 10 at 57:19 “Specifically re: para – can para of close to intestine or colon or anywhere in that area cause gastro problems?
Q 11 at 58:34 “Please weigh in on controversy of screening for patients/families with incidental SDHA mutations.”
Q 12 at 1:00:39 “I’m the first in my family to have multiple H&N paras, & a FH mutation. Since my genetic testing, two family members also tested positive for the FH mutation. Should they get a H&N & abdomen MRIs & metanephrines? One had an incidental finding of bilateral kidney cysts. It’s difficult because despite sharing their genetic testing results, and my history, their doctors don’t see the need for MRI/CT. Thank you!”
Q 13 at 1:02:01 “What are the treatment options for patients with inoperable Paragangliomas, such as situated in the bifurcation of the Carotid artery? And whatever are the long term side effects of these treatments?”
Q 14 at 1:05:23 “Based on the initial screening guidelines, what would you recommend for an asymptomatic patient with an SDHD mutation whose MRIs have shown very small, questionable nodules that could mimic enlarged lymph nodes in the head and neck? Would you recommend scans every year, or every 2-3 years?”
Q 15 at 1:07:28 “I had a pheochromocytoma from ages 13-27. It was removed at age 27. I nearly died, now at age 58 diagnosed with paraganglioma. I received radiation therapy and am still awaiting the results. Will I get such a paraganglioma again in my lifetime?”
Q 16 at 1:08:17 “How to manage the metastasis PPGLs with no detectable lesions or mets? Does PRRT help? Would you recommend a DOTATATE scan for this patient if one has not been performed?”
Q 17 at 1:11:14 “For plasma biochemical testing: Is it critical that a patient rest in a supine position before blood is drawn?”
Q 18 at 1:12:32 “Will research regarding IVF ever be considered “preventative” for those with a confirmed mutation?”
Q 19 at 1:13:33 “Do all patients with a pheo or para have a higher chromogranin A level?”
Q 20 at 1:15:18 “Are the SDHB and SDHD genetic mutations more similar than SDHA and SDHC?”
Q 21 at 1:17:03 “Why should the vocal cord be immobile?” (references material presented at 27:48)
Q 22 at 1:19:07 “Is altitude the only thing that increases risk for SDHB patients, or are there other factors that can increase the risk of tumor growth?”
Q 23 at 1:20:27 “I had metastatic disease and underwent removal of the tumor, with residual disease in bone. After undergoing treatment with Lutathera a follow-up PET scan shows those spots are more active. Are there any further treatment recommendations, or is everything at this point experimental and screening?”
Q 24 at 1:23:30 “Could you help define ‘metastatic paraganglioma?’ If I have multiple head and neck tumors, is that considered metastatic?”
Q 25 at 1:24:57 “If a patient has metastatic pheo and then a relative has bilateral pheo and a pituitary tumor but both show no known gene when tested, is it likely that there is an unknown gene involved?”
Q 26 at 1:26:22 “Could you please explain why hypertension is NOT part of the signs and symptoms of pheo para?”